Menu
Tumor medication
Common Medications
{{ variable.name }}
Golimumab (golimumab) instruction manual
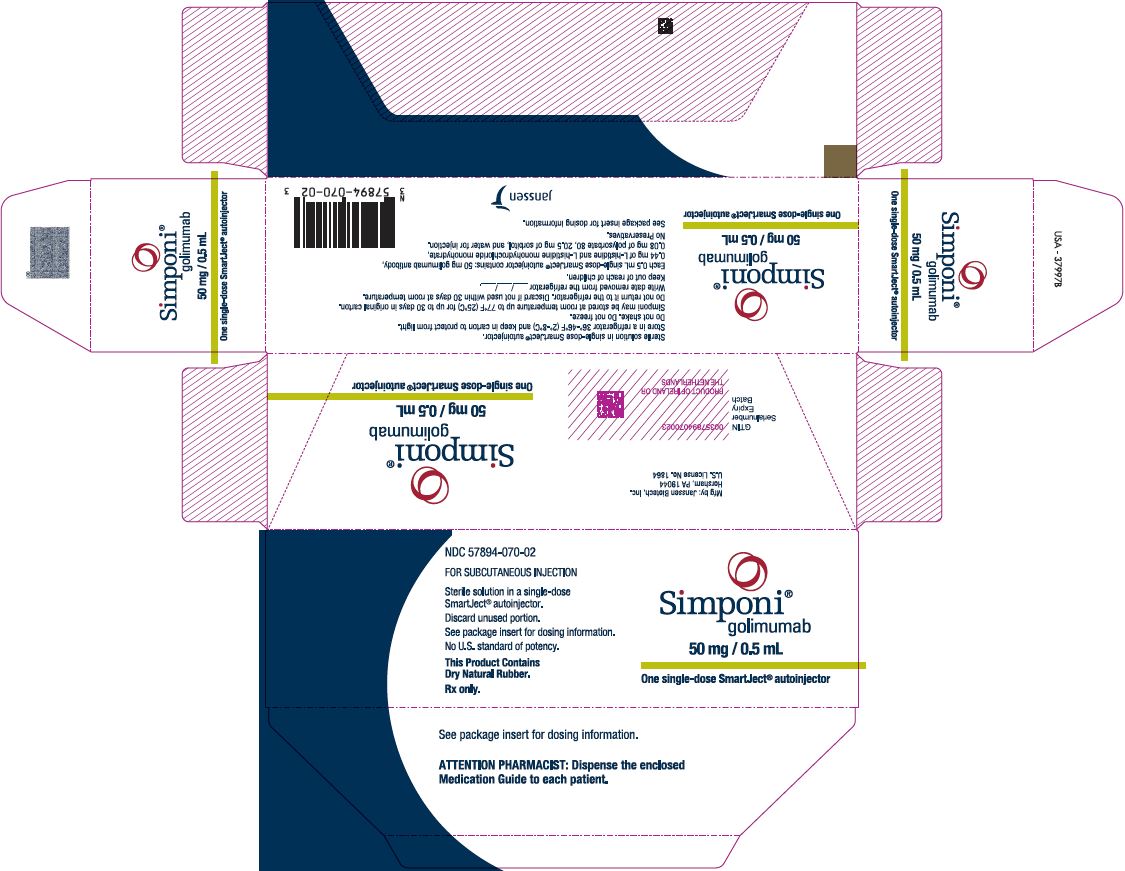
Common name: golimumab injection
Trade name: Xinproni
Full names: golimumab, golimumab injection, Xinpi, golimum ab, simponi
Indications:
Rheumatoid arthritis:
This product combined with methotrexate (MTX) is suitable for the treatment of adult patients with moderate to severe active rheumatoid arthritis who have failed to respond to disease-modifying antirheumatic drugs (DMARDs) including MTX.
This product combined with MTX (methotrexate) has been proven to reduce the incidence of progression of joint damage (detected by X-ray) and improve physical function.
Ankylosing spondylitis:
This product is suitable for the treatment of adult patients with active ankylosing spondylitis.
Usage and dosage:
Rheumatoid arthritis: 50 mg of this product, administered once a month. Subcutaneous injection. This product should be used in combination with MTX (methotrexate).
Ankylosing spondylitis: 50 mg of this product, administered once a month. Subcutaneous injection. Available data indicate that patients with rheumatoid arthritis and ankylosing spondylitis typically recover within 12-14 weeks of treatment (3-4 After 1 dose) clinical response was obtained. Patients who do not develop evidence of treatment benefit within this time period should reconsider continuing treatment.
Adverse reactions:
The most common adverse drug reaction is upper respiratory tract infection.
The most serious adverse drug reactions include serious infections (including sepsis, infectious pneumonia, tuberculosis, invasive fungal infections and opportunistic infections), demyelinating diseases, hepatitis B reactivation, congestive heart failure, autoimmune diseases (lupus-like syndrome), hematological reactions, severe systemic hypersensitivity reactions (including anaphylaxis), vasculitis, lymphoma and leukemia.
Contraindications:
Hypersensitivity to the active ingredient or any excipients.
Active tuberculosis or other severe infections such as sepsis and opportunistic infections.
Moderate or severe heart failure (NYHA class III/MV).
Precautions:
Infections: Infections (including tuberculosis) must be closely monitored before, during and after treatment with this product. Because elimination of this product may take up to 5 months, patients should continue to be monitored during this period. This product should not be used again if the patient develops severe infection or sepsis. This product should not be used in patients with clinically severe, active infection. Caution should be exercised when considering the use of this product in patients with chronic infections or a history of recurrent infections. Patients should be informed of potential risk factors for infection and should avoid exposure to potential risk factors for infection. Patients taking TNF blockers are more likely to develop serious infections. Bacterial infections (including sepsis and infectious pneumonia), mycobacterial infections (including tuberculosis), invasive fungal infections, and opportunistic infections, including infections resulting in death, have been reported in patients treated with this product. Patients often present with disseminated rather than homofocal infection. Patients combined with immunotherapeutic therapy have experienced some of the above-mentioned serious infections. In addition, these patients often have underlying diseases, making them more susceptible to infections. Patients who develop new infections while receiving this product should be closely monitored and have a thorough diagnostic evaluation performed. If a patient develops a new serious infection or sepsis, AVICIN should be discontinued and appropriate antimicrobial or antifungal therapy initiated until the infection is controlled.
Tuberculosis: Tuberculosis has been reported in patients receiving this product. In most reports, TB is extrapulmonary and presents as focal or disseminated. All patients should be evaluated for active and inactive ("latent") tuberculosis before initiating treatment with this product. This assessment should include detailed medical history: personal history of TB, possible past exposure to TB, and past and/or current immunosuppressive treatment. Appropriate screening (ie, tuberculin skin test or blood test and chest X-ray) should be performed on all patients or local recommendations may be followed. Prescribers should be aware of the risk of false-negative tuberculin skin test results, particularly in critically ill or immunocompromised patients. Treatment with this product should not be started if active tuberculosis is diagnosed. If latent tuberculosis is suspected, a specialist in tuberculosis treatment should be consulted. In all of the following situations, the benefits and risks of treatment with this product should be carefully weighed. If inactive ("latent") tuberculosis is diagnosed, anti-tuberculosis treatment must be initiated before starting treatment with this product, and local recommendations must be followed. In patients who test negative for latent tuberculosis but have several or significant risk factors for tuberculosis, antituberculosis therapy should be considered before initiating treatment with tacitabine. The decision on whether to start anti-tuberculosis treatment for the above-mentioned patients can be made only after consulting a tuberculosis treatment specialist and considering the risk of latent tuberculosis infection and the risk of anti-tuberculosis treatment. For patients with a past history of latent tuberculosis or active tuberculosis and who are not sure that they have received an adequate course of treatment, anti-tuberculosis treatment should also be considered before starting treatment with this product. Active tuberculosis has been reported in patients receiving this product during and after treatment for latent tuberculosis. Patients receiving this product (including patients with negative latent tuberculosis test results, patients receiving treatment for latent tuberculosis, and patients who have been previously treated for tuberculosis infection) should be closely monitored for signs and symptoms of active tuberculosis. All patients should be informed that they should seek medical attention if they develop signs/symptoms suggestive of tuberculosis (e.g., persistent cough, wasting/weight loss, low-grade fever) during or after treatment with this product.
Hepatitis B reactivation: Hepatitis B relapse has occurred in chronic carriers of hepatitis B virus (i.e., surface antigen-positive persons) treated with TNF blockers, including this product, and in some cases fatal outcomes have occurred. Patients should be tested for HBV infection before treatment with this product. For patients who test positive for HBV infection, it is recommended to consult a hepatitis B treatment specialist. HBV carriers who require treatment with this product should be appropriately evaluated and closely monitored for signs and symptoms of active HBV infection before starting treatment, during treatment, and for several months after the end of treatment. There are insufficient data on combined antiviral therapy to prevent HBV reactivation and TNF blocker therapy in HBV carriers. Patients who experience HBV reactivation should discontinue this product and initiate effective antiviral therapy and appropriate supportive care.
Malignant neoplasms and lymphoproliferative disorders: The potential role of TNF blocker therapy in the development of malignancies is unclear. Based on current knowledge, the possible risk of developing lymphoma, leukemia or other malignancies in patients treated with TNF blockers cannot be excluded. Caution should be exercised when considering TNF blockade therapy in patients with a history of malignancy or when considering continued TNF blockade therapy in patients who have developed malignancy.
Pediatric malignant tumors: This product has not been approved for use in children and adolescent patients in China. However, relevant foreign research data and post-marketing data indicate that lymphoma and other malignant tumors (some of which are fatal) have been reported in severely ill infants and adolescent patients when treated with TNF blockers including this product. Post-marketing, cases of malignancy, some of which were fatal, have been reported in children, adolescents, and young adults (up to 22 years of age) treated with TNF blockers (age ≤18 years at initiation of treatment). Approximately half of the cases are lymphoid neoplasms, and the remainder manifest as a variety of different malignancies, including rare malignancies often associated with immunosuppression. The risk of malignancy in children and adolescents treated with TNF blockers cannot be excluded.
Lymphoma and leukemia: In controlled clinical trials of all TNF blockers (including this product), more cases of lymphoma were observed in the anti-TNF treatment group than in the control group. During Phase IIb and Phase III clinical trials in rheumatoid arthritis and ankylosing spondylitis, the incidence of lymphoma in patients treated with this product was higher than expected in the general population. Leukemia has been reported in patients receiving this product. Rheumatoid arthritis patients with long-term inflammatory activity have an increased risk of lymphoma and leukemia compared with the general population. Rare post-marketing cases of hepatosplenic T-cell lymphoma (HSTCL) have been reported in patients treated with other TNF blockers. This rare type of T-cell lymphoma is highly aggressive and often leads to death. Most cases occur in adolescents and young adult males, and almost all cases are in patients with inflammatory bowel disease who have received azathioprine (AZA) or 6-mercaptoin (6-MP) in combination with TNF blockers. The potential risks of combining AZA or 6-MP with this product should be carefully considered. The risk of developing hepatosplenic T-cell lymphoma in patients treated with TNF blockers cannot be excluded.
Other malignancies other than lymphoma: In the phase IIb and phase III controlled studies of clinical trials in rheumatoid arthritis, ankylosing spondylitis and other adult patients, the incidence rate of non-lymphoma malignancies (except non-melanoma skin cancer) in the treatment group was similar to that in the control group.
Colon dysplasia/colon cancer: It is not known whether treatment with this product affects the risk of colon dysplasia or colon cancer. Patients with ulcerative colitis who are at increased risk for colonic dysplasia or colon cancer (for example, patients with long-standing ulcerative colitis or primary sclerosing cholangitis) or who have a history of colonic dysplasia or colon cancer should be screened before treatment and periodically throughout the course of their disease. Specific evaluation includes colonoscopy and biopsy in accordance with local recommendations. For patients with newly diagnosed colonic dysplasia receiving treatment with this product, the risks and benefits of the individual patient must be carefully weighed and whether to continue treatment.
Skin Cancer: Melanoma and Merkel cell carcinoma have been reported in patients receiving TNF blockers, including this product. Regular skin examinations are recommended (especially for patients with risk factors for skin cancer).
Congestive heart failure: Worsening and new cases of congestive heart failure have been reported during treatment with TNF blockers (including this product), and some cases have fatal outcomes. In a clinical trial using another TNF blocker, worsening of congestive heart failure and increased mortality due to congestive heart failure were observed. This product has not been studied in patients with congestive heart failure. Patients with mild heart failure (NYHA class I/II) should use this product with caution. Patients should be monitored closely and if new or worsening symptoms of heart failure occur, this product must be discontinued.
Anaphylaxis: Post-marketing reports of severe systemic hypersensitivity reactions, including anaphylaxis, have been reported in patients treated with this product. Some of these severe systemic hypersensitivity reactions have occurred after first use of this product. If anaphylaxis or other serious allergic reactions occur, discontinue use of this product immediately and initiate appropriate treatment.
Storage:
Store at 2℃~8℃ away from light.
Freezing is strictly prohibited.
Mechanism of action:
The drug selectively binds to soluble and membrane-bound TNFα in in vitro experiments and shows the following effects:
(1) Inhibits the binding of TNFα to TNF receptors.
(2) Stimulate the production of fibroblasts or endothelial cytokines (IL-6, IL-8, G-CSF, GM-CSF) and adhesion molecules (E-selectin, ICAM-1, VCAM) in endothelial cells through TNFα stimulation -1) In mice.
This product significantly delayed the onset of arthritis in human TNFα transgenic mice and significantly inhibited histopathological changes in joints.
Safety and efficacy:
In order to explore the efficacy and nursing experience of using golimumab in the treatment of ankylosing spondylitis, the clinical data of 40 patients with ankylosing spondylitis treated with golimumab were selected. The BASDAI, VAS score, morning stiffness time, Schber test, thoracic expansion, C-reactive protein (CRP), erythrocyte sedimentation rate (ESR) and nursing satisfaction before and after treatment were statistically analyzed. Results: There were significant differences in BASDAI, pain VAS score, morning stiffness time, Schber test, thoracic expansion, CRP, and ESR before golimumab treatment and after 6 weeks and 12 weeks of treatment in patients with ankylosing spondylitis (P0.05). The patients' quality of life score, SAS score, and nursing satisfaction score after treatment were significantly better than before treatment, and the difference was significant (P<0.05). Conclusion: Golimumab has obvious effects in the treatment of ankylosing spondylitis. At the same time, through appropriate nursing intervention, it can significantly improve patients' quality of life and nursing satisfaction.